By Joke Kujenya
A SILENT epidemic is wreaking havoc on the health of millions worldwide.
It is called High Blood Pressure (hypertension/HPB), often undetected until severe damage is done, affects over 1.2 billion people globally.
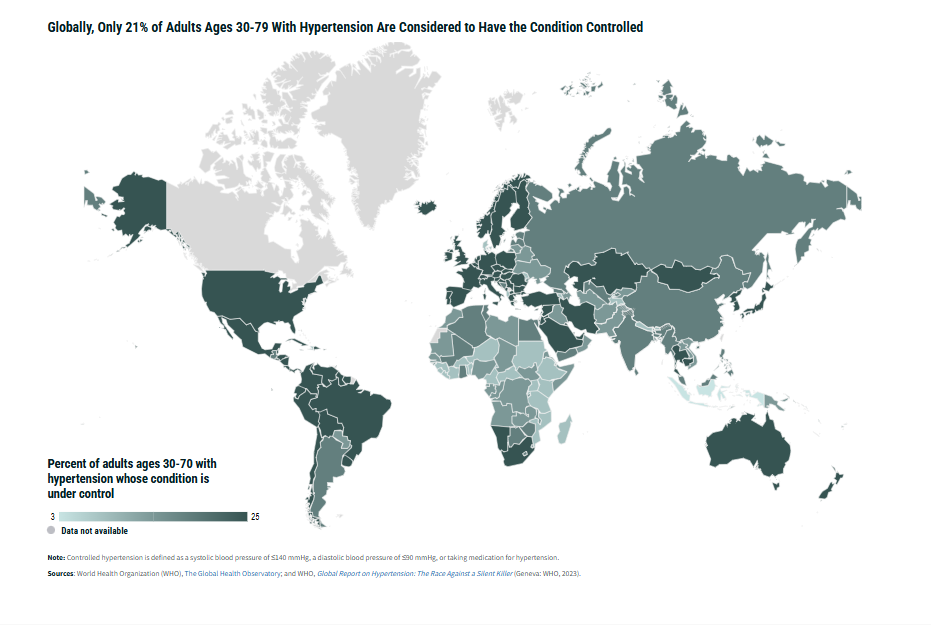
However, despite advancements in healthcare, reports say only 21% of adults aged 30-79 who suffer from this condition have it under control.
In both developing and developed nations, inadequate access to Primary Health Care (PHC) is one of the main barriers to effectively managing this deadly disease.
Furthermore, information says cardiovascular disease causes 17 million deaths globally each year, accounting for nearly one-third of all deaths.
Hypertension complications contribute to 9.4 million of these death and linked to 45% of heart disease deaths and 51% of stroke-related deaths worldwide.
A Growing Global Crisis
Hypertension is reported to be a leading cause of heart disease, stroke, and kidney failure, claiming millions of lives every year.
Sadly, Primary Health Care (PHC), which is the first point of contact for most people seeking medical attention, has proven critical in preventing and managing chronic diseases like hypertension.
Yet, global disparities in access to PHC are worsening the crisis.
In fact, 50% of the world’s population still lacks access to basic healthcare services, leaving millions vulnerable to untreated and uncontrolled blood pressure.
Also, in countries with low-income or underdeveloped healthcare systems, PHC services struggle to meet demand.
The World Health Organization (WHO) estimates that scaling up access to quality PHC could avert 60 million deaths by 2030 and increase global life expectancy by up to 3.7 years.
But, achieving this requires an additional investment of $200 to $328 billion annually to strengthen PHC systems, especially in low- and middle-income countries.
Impact in Low-Income Nations
Moreover, according to 2024 World Population Data Sheet, the burden of hypertension disproportionately affects low- and middle-income nations, where healthcare infrastructure is often underdeveloped or severely underfunded.
Countries in sub-Saharan Africa, for example, face a growing prevalence of high blood pressure due to rapid urbanization, poor diets, and lack of access to routine health screenings.
In Ghana, nurses handle 80% of healthcare services, including hypertension diagnosis and management. Unfortunately, a chronic shortage of professional health workers significantly undermines their ability to provide adequate care.
While Ghana’s government implemented a national strategy to boost its nursing workforce between 2007 and 2011, resulting in a 640% increase in nurses by 2018, the country still struggles to meet the growing demand for healthcare services, especially in rural areas where hypertension remains undiagnosed and untreated for years.
The Role of Community Health Workers
In addition to professional nurses, many low-income countries are heavily reliant on Community Health Workers (CHWs).
These individuals, often trained to provide preventive and basic curative care, are a critical part of PHC systems.
Also, their role is even more vital in rural and underserved areas, where health facilities may be sparse, and travel to a hospital or clinic can take hours.
CHWs are often the first point of contact for those suffering from hypertension, providing basic health checks, advising on lifestyle changes, and referring patients to higher levels of care if needed.
However, despite their critical role, many CHWs operate as volunteers, with little training or formal accreditation.
This lack of consistent professional support further contributes to the gap in quality care for hypertension patients, who may require more specialized attention that a CHW cannot provide.
This has led to a growing call for governments to professionalize and expand CHW programs to enhance their capacity to deliver essential services, including hypertension management.
PHC Around the World: Comparing Approaches
Globally, countries are taking varied approaches to tackling hypertension through primary health care.
South Africa, a country facing high burdens of both infectious diseases like HIV and tuberculosis, and noncommunicable diseases like hypertension, has integrated hypertension management into its PHC framework.
This approach ensures that those diagnosed with high blood pressure are regularly monitored and receive treatment through a network of district health systems.
In contrast, the United Kingdom’s National Health Service (NHS) emphasizes a more comprehensive approach to PHC.
Its services include regular health screenings for hypertension, preventive measures, and treatment through a well-established network of general practitioners, nurses, and allied health professionals.
The NHS ensures patient participation, enabling individuals to take part in monitoring and managing their health conditions.
Thailand offers another perspective on the PHC approach, with rural and urban settings defining the scope of services offered.
In rural areas, district health systems provide comprehensive care that includes hypertension screenings and treatment, while urban populations often rely on public and private hospitals for primary care.
Despite these efforts, urbanization and migration patterns are stressing healthcare systems in Thailand, leaving many urban poor without access to necessary hypertension care.
The Strain on Health Workers
One of the greatest barriers to controlling hypertension worldwide is the shortage of skilled health workers.
Nurses, physicians, and other healthcare providers are often overwhelmed by the sheer number of patients needing care.
This is especially true in regions where healthcare professionals are scarce and where the migration of healthcare workers to wealthier countries for better pay leaves a vacuum of expertise.
The ongoing migration of health professionals from low- and middle-income countries to more developed regions exacerbates the crisis.
Countries such as Ghana and Nigeria, already grappling with staffing shortages, face the added challenge of losing trained nurses and doctors to wealthier nations, where wages and working conditions are more attractive.
This further reduces the availability of qualified personnel to treat hypertension and other chronic conditions in under-resourced areas.
Investments in PHC: A Lifesaving Solution
To combat the global hypertension crisis, substantial investments are needed to bolster primary health care systems worldwide.
Furthermore, the WHO has urged governments to invest in both infrastructure and human resources to make healthcare more accessible and responsive to their populations’ needs.
Additionally, improving training, recruitment, and retention of healthcare workers is crucial to ensure a steady workforce capable of managing diseases like hypertension.
Countries must also focus on integrating chronic disease management into existing PHC services.
This will allow health workers to routinely screen for hypertension, ensure that medications are available, and provide follow-up care.
In doing so, millions of lives can be saved through early detection, lifestyle interventions, and medical treatment, averting the serious consequences of untreated high blood pressure.
At the World Health Assembly in May 2024, global leaders recognized the need for a whole-of-society approach to PHC.
This involves not just health professionals, but also the active participation of communities, families, and individuals in their own care.
Engaging people in monitoring their blood pressure and making informed health decisions is key to reducing the global burden of hypertension.
Ticking Time Bomb
Hypertension remains a ticking time bomb in global health, the report warns.
Without widespread access to primary health care, millions are left vulnerable to preventable complications such as heart disease, stroke, and kidney failure.
Investing in PHC, particularly in low- and middle-income countries, can avert millions of unnecessary deaths and improve the quality of life for millions more.
Addressing health workforce shortages and ensuring the availability of essential medicines and diagnostics are critical to turning the tide on this growing global health challenge.
At JKNewsMedia, our dedication to delivering reliable news and insightful information to our cherished readers remains unwavering. Every day, we strive to provide you with top-notch content that informs and enlightens. By donating to JKNewsMedia, you directly contribute to our mission of delivering quality journalism that empowers and informs. Your support fuels our commitment to bringing you the latest updates and in-depth analysis. Let's continue to uphold the highest standards of journalism and serve our community with integrity and dedication. Thank you for being a part of the JKNewsMedia family and for your ongoing support.





