By Joke Kujenya
CERVICAL CANCER remains a silent killer, claiming the lives of hundreds of thousands of women globally each year.
Despite medical advancements, many women—especially in low- and middle-income countries—continue to die due to late detection and limited access to preventive healthcare.
The disease, primarily caused by persistent infection with the Human Papillomavirus (HPV), can be prevented through vaccination, regular screening, and early treatment.
Yet, millions remain unaware of the risks until it is too late.
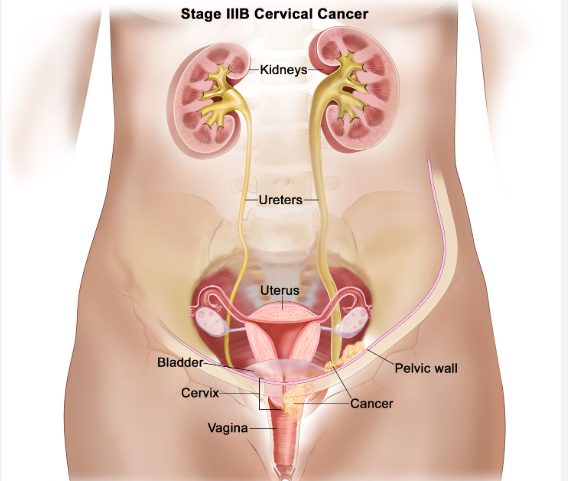
Women who develop cervical cancer often have no symptoms in its early stages.
By the time they experience abnormal bleeding, pelvic pain, or unusual discharge, the disease may have already advanced. HPV, the main culprit, spreads through sexual contact, and while many infections clear naturally, some linger and trigger dangerous cell changes in the cervix.
Additional risk factors include early sexual activity, multiple sexual partners, smoking, and weakened immunity—particularly in women living with HIV.
In Nigeria and other developing nations, the absence of widespread HPV vaccination programmes and limited access to regular screenings exacerbates the problem.
Many women never undergo a Pap smear or HPV test due to cost, cultural barriers, or lack of awareness.
According to the World Health Organization (WHO), women living with HIV are six times more likely to develop cervical cancer, yet only a fraction receive timely screening and care.
Medical experts stress that prevention is key.
The HPV vaccine, ideally administered to girls aged 9–14, offers significant protection against the virus strains most likely to cause cancer.
Regular screenings can detect precancerous changes early, allowing for prompt intervention.
Pap smears and HPV tests remain the most effective tools for early detection, yet many health systems fail to prioritise them, leaving women vulnerable.
For those diagnosed, treatment depends on the stage of the disease.
Surgery, radiation therapy, and chemotherapy are common approaches, while newer treatments like immunotherapy show promise in advanced cases.
Survivors often endure physical and emotional trauma, but access to quality healthcare can significantly improve their outcomes.
Alternative remedies, such as the herbal drink called Jigsimur, have gained popularity among some seeking preventive and complementary treatments.
While proponents claim it boosts immunity and repairs damaged cells, experts caution against relying solely on herbal solutions without medical oversight.
Cervical cancer does not only affect women. HPV can also cause cancers in men, including penile, anal, and throat cancers.
Despite this, public health campaigns often focus exclusively on women, leaving many men unaware of the risks.
Efforts to eliminate cervical cancer by 2030 are underway, with global health organisations pushing for universal HPV vaccination, increased screening, and better treatment access.
Governments must prioritise these interventions to close the gap and protect future generations.
However, raising awareness, ensuring early detection, and expanding prevention programmes can turn the tide against cervical cancer.
The WHO reiterates that every woman deserves a chance to live free from a disease that is largely preventable.
Meanwhile, the battle against cervical cancer is far from over, but with collective action, it can be won.